Reticulospinal tract
This article has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these template messages)
|
The reticulospinal tracts (also known as descending or anterior reticulospinal tracts) are extrapyramidal motor tracts that descend from the reticular formation[1] in two tracts to act on the motor neurons supplying the trunk and proximal limb flexors and extensors. The reticulospinal tracts are involved mainly in locomotion and postural control, although they do have other functions as well.[2]
The reticulospinal tracts are one of four major cortical pathways to the spinal cord for musculoskeletal activity. The reticulospinal tracts work with the other three pathways to give a coordinated control of movement, including fine movement. The four pathways can be grouped into two main system pathways – a medial system and a lateral system. The medial system includes the reticulospinal pathway and the vestibulospinal pathway, and this system provides control of posture. The corticospinal and the rubrospinal tract pathways belong to the lateral system which provides fine control of movement.[1]
This descending tract is consists of two parts: the medial (or pontine) and lateral (or medullary) reticulospinal tracts.
The reticulospinal tracts are involved in coordinating the activity of skeletal muscle (including tone and reflexes) by influencing the alpha and gamma motor neurons that innervate them. The tracts are involved in in reciprocal inhibition of antagonist muscles: the tract ensure that contraction of specific flexors is accompanied by relaxation of their antagonist extensors - and vice versa. In collaboration with the lateral vestibulospinal tract, the tracts participate in maintaining balance and adjusting posture: this - as well as maintaining muscle tone - is a pre-requisite enabling voluntary movements to be performed properly.[3]
The neurons giving rise to the reticulospinal tracts receive (and integrate) afferents from the premotor cortex, supplementary motor area, basal nuclei, cerebellum, substantia nigra, and red nucleus, as well as from other areas of the reticular formation.[3]
Medial reticulospinal tract
[edit]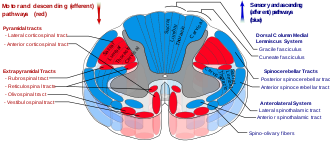
The medial reticulospinal tract or pontine reticulospinal tract arises from the pontine reticular formation, which consists of the oral and caudal pontine reticular nuclei. The tract descends through the ipsilateral anterior funiculus of the spinal cord, projecting to all levels of the spinal cord.[3] It terminates in the laminae VII and VIII of the spinal cord.[citation needed]
It terminates by synapsing with interneurons and gamma motor neurons to exciting extensors and inhibiting flexors of the axial and proximal limb musculature (opposing the effects of the lateral reticulospinal tract). Many axons of this tract synapse with reflex propriospinal interneurons that in turn synapse with motor neurons of these muscles. A few axons also form inhibitory synapses with first-order sensory neurons innervating muscle spindles, thus inhibiting stretch reflex to enable smoother voluntary movements.[3]
Lateral reticulospinal tract
[edit]The lateral reticulospinal tract or medullary reticulospinal tract arise from the medullary reticular formation (which consists of the gigantocellular and ventral reticular nuclei[3] - with the greatest contribution from the gigantocelular nucleus[citation needed]).[3] In the spinal cord, it descends mostly through the ipsilateral[3] anterior part of the lateral funiculus.[citation needed] It projects to all levels of the spinal cord.[3] The tract terminates mostly in laminae VII of the spinal cord, with some fibers terminating in laminae IX.[citation needed]
The tract terminates primarily by synapsing with the interneuron of the intermediate zone of spinal grey matter. It excites flexors and inhibits extensors of the axial and proximal limb musculature (opposing the effects of the medial reticulospinal tract). Some axons of the tract synapse with lower motor neurons of the distal limb musculature which then counteract the action of lower motor neurons innervating the axial extensors and promote those innervating limb flexors.[3]
Clinical significance
[edit]The reticulospinal tracts provide a pathway by which the hypothalamus can control sympathetic thoracolumbar outflow and parasympathetic sacral outflow.[citation needed]
Two major descending systems carrying signals from the brainstem and cerebellum to the spinal cord can trigger automatic postural response for balance and orientation: vestibulospinal tracts from the vestibular nuclei and reticulospinal tracts from the pons and medulla. Lesions of these tracts result in profound ataxia and postural instability.[4]
Physical or vascular damage to the brainstem disconnecting the red nucleus (midbrain) and the vestibular nuclei (pons) may cause decerebrate rigidity, which has the neurological sign of increased muscle tone and hyperactive stretch reflexes. Responding to a startling or painful stimulus, both arms and legs extend and turn internally. The cause is the tonic activity of lateral vestibulospinal and reticulospinal tracts stimulating extensor motoneurons without the inhibitions from rubrospinal tract.[5]
Brainstem damage above the red nucleus level may cause decorticate rigidity. Responding to a startling or painful stimulus, the arms flex and the legs extend. The cause is the red nucleus, via the rubrospinal tract, counteracting the extensor motorneuron's excitation from the lateral vestibulospinal and reticulospinal tracts. Because the rubrospinal tract only extends to the cervical spinal cord, it mostly acts on the arms by exciting the flexor muscles and inhibiting the extensors, rather than the legs.[5]
Damage to the medulla below the vestibular nuclei may cause flaccid paralysis, hypotonia, loss of respiratory drive, and quadriplegia. There are no reflexes resembling early stages of spinal shock because of complete loss of activity in the motorneurons, as there is no longer any tonic activity arising from the lateral vestibulospinal and reticulospinal tracts.[5]
References
[edit]- ^ a b Squire L (2013). Fundamental neuroscience (4th ed.). Amsterdam: Elsevier/Academic Press. pp. 631–632. ISBN 978-0123858702.
- ^ FitzGerald MT, Gruener G, Mtui E (2012). Clinical Neuroanatomy and Neuroscience. Philadelphia: Saunders Elsevier. p. 192. ISBN 978-0702037382.
- ^ a b c d e f g h i Patestas, Maria A.; Gartner, Leslie P. (2016). A Textbook of Neuroanatomy (2nd ed.). Hoboken, New Jersey: Wiley-Blackwell. pp. 309–310. ISBN 978-1-118-67746-9.
- ^ Pearson, Keir G; Gordon, James E (2013). "Chapter 41 / Posture". In Kandel, Eric R; Schwartz, James H; Jessell, Thomas M; Siegelbaum, Steven A; Hudspeth, AJ (eds.). Principles of Neural Science (5th ed.). United States: McGraw-Hill. The Brain Stem and Cerebellum Integrate Sensory Signals for Posture, p. 954. ISBN 978-0071390118.
- ^ a b c Michael-Titus et al (2010b), Box 9.5 Decorticate and decrebrate regidity, p. 172